Do I Need Prior Authorization for Free Incontinence Supplies with Molina?
Summary
- Molina generally does not require prior authorization for incontinence supplies in Washington or Idaho, as long as they are obtained through an approved supplier.
- Prior authorization may become necessary if supplies come from a non-approved provider and under certain other conditions.
- Understanding Molina’s prior authorization rules helps avoid unexpected denials of incontinence supplies.
No, Molina does not require prior authorization to get free incontinence supplies, as long as those supplies are from the preferred provider network. This is true for Molina in Washington and Molina in Idaho.
 Here’s why, with helpful details explaining:
Here’s why, with helpful details explaining:
- What prior authorization is
- When prior authorization is not required for free incontinence supplies with Molina
- When Molina requires prior authorization
- How to find out more about free incontinence supplies with Molina
This 3-minute guide walks you through the what, why, and how of prior authorizations for Molina, so you can figure out what next steps may be necessary for you to get free incontinence supplies with Molina.
If you need help from a Medicaid expert in Washington, Idaho, or Oregon, contact MyMedSupplies (or call 888-441-1312).
We help folks like you every day, and we’re ready to walk you through the process with care, compassion, and expertise.
What Is Prior Authorization?
 Prior authorization means Molina has to approve the medical care or provision before it’s provided or received. In other words, Molina needs to decide whether the care or equipment is necessary before approving and covering it.
Prior authorization means Molina has to approve the medical care or provision before it’s provided or received. In other words, Molina needs to decide whether the care or equipment is necessary before approving and covering it.
So, if prior authorization is a requirement for coverage, failing to get this prior authorization can result in no coverage with Molina.
Crucially, Molina does not require prior authorization for a lot of care and medical supplies. Understanding when and how prior authorizations can come into play with incontinence supplies is essential for those who want to leverage the full extent of their coverage properly.
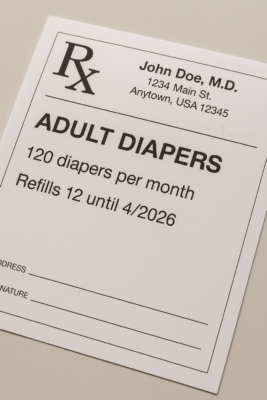
When Prior Authorization Is Not Required for Free Incontinence Supplies with Molina?
Prior authorization for incontinence supplies through Molina is NOT generally required when:
 Your supplies come from an approved supplier: Molina works with specific providers and suppliers, including My Med Supplies. When you work with one of these approved suppliers, prior authorizations are not required. If, however, you are trying to get diapers, briefs, pull-ups, and other incontinence supplies from a non-approved provider, it may be necessary to get prior authorization for coverage.
Your supplies come from an approved supplier: Molina works with specific providers and suppliers, including My Med Supplies. When you work with one of these approved suppliers, prior authorizations are not required. If, however, you are trying to get diapers, briefs, pull-ups, and other incontinence supplies from a non-approved provider, it may be necessary to get prior authorization for coverage.- The specific supplies you need are covered: All types, brands, and styles of incontinence supplies are not necessarily covered by Molina. There are specific definitions associated with different types of incontinence supplies; therefore, only some brands are covered. If you need different brands that fall outside of the standard definitions and approved supplies, again, prior authorization may be needed.
- The amount you need exceeds the limits: If the monthly limits won’t cut it, meaning ~200 diapers per month is not enough, then prior authorization may be required to approve the higher limits for your needs.
If you’re just getting started with incontinence supplies via Molina, it can be difficult to know what you need and whether a prior authorization is required for your circumstances.
That’s where My Med Supplies comes in. We can help you figure out what you need, whether prior authorizations are required in your case, and how to move forward.
Simply email us or call 888-441-1312 to talk to a real person, who cares and who is ready to help you get free incontinence supplies with Molina in WA or ID.
When Does Molina Require Prior Authorizations?
 Along with the details provided above, Molina can also require prior authorization for in-home care, physical therapy, and specialized medical equipment, like (but not limited to):
Along with the details provided above, Molina can also require prior authorization for in-home care, physical therapy, and specialized medical equipment, like (but not limited to):
- Walkers, including standard walkers, as well as 2-wheel, 3-wheel, and 4-wheel walkers
- Wheelchairs, including manual and motorized varieties
In most cases, prior authorizations are focused on care, rather than medical equipment or supplies.
When prior authorizations are required, healthcare providers must handle the requests with Molina (individuals cannot pursue prior authorizations on their own).
Regardless, however, it’s generally best to double-check the potential need for prior authorization with an expert, especially if your medical supply needs don’t fit the limits established by Molina or state Medicaid.
How to Find Out More About Free Incontinence Supplies with Molina
Many folks eligible for free incontinence supplies through Molina will not need to obtain prior authorization to get these items. Others may need to, and the best way to know what applies to you is to contact an expert at MyMedSupplies.
Simply email us or call 888-441-1312 to talk to a real person who is ready to help you get free incontinence supplies with Molina in WA, OR, or ID.
We have helped countless folks just like you get free incontinence supplies through Molina in WA and ID, and we’re ready to help you now.