What If Medicaid Denies My Request for Incontinence Supplies?
Medicaid denials for incontinence supplies can be discouraging, especially when you or someone you care for has a genuine need. The good news is that these denials don’t automatically mean you are ineligible. In many cases, it means something in the paperwork, diagnosis, and/or documentation needs to be corrected.
 Here’s why and:
Here’s why and:
- Common Reasons Medicaid Denies Incontinence Supply Requests
- What to Do First After a Denial
- How the Medicaid Appeal Process Works
- Doctor Documentation Fixes That Often Lead to Approval
- Resubmitting Your Request Successfully
- Washington, Oregon & Idaho Medicaid Notes
- When a Denial Doesn’t Mean “No”
- How MyMedSupplies Helps After a Denial
- When Medicaid Denies Diaper Coverage: Next Steps
Remember, Medicaid can come with some hoops to jump through, and thousands of Medicaid beneficiaries in Washington, Oregon, and Idaho successfully receive free adult diapers, pull-ups, and related incontinence supplies every month.
So, if your request was denied, don’t take that as the final word on the matter. Explore your options and take action with the support of this guide or professionals, like the experts at MyMedSupplies.
5 Common Reasons Medicaid Denies Incontinence Supply Requests
Medicaid denials are usually based on administrative grounds, not medical reasons. With that, some of the most frequent causes of these denials are as follows.
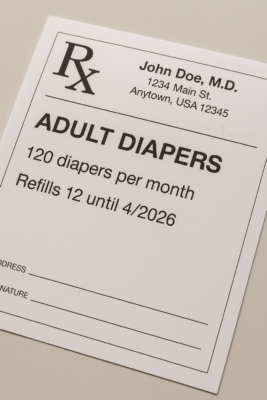
1. Missing or Incomplete Prescription
Medicaid requires a valid prescription (or written order) from a licensed healthcare provider. Your request may be rejected if the prescription:
- Lacks a diagnosis code
- Does not specify product type
- Is missing quantity or frequency details
- Is expired.
2. Diagnosis Does Not Support Medical Necessity
 Medicaid must see documentation that incontinence supplies are medically necessary, not simply for convenience. If the diagnosis is vague (e.g., “bladder issues”) or unrelated, the request may be denied.
Medicaid must see documentation that incontinence supplies are medically necessary, not simply for convenience. If the diagnosis is vague (e.g., “bladder issues”) or unrelated, the request may be denied.
3. Quantity Exceeds State or Plan Limits
Each Medicaid program and managed care organization sets monthly quantity caps. Requests that exceed standard limits without justification are commonly denied.
4. Prior Authorization Was Not Submitted (or Not Approved)
Some plans require prior authorization before supplies are covered. If authorization was not requested or was submitted incorrectly, coverage may be denied.
5. Member Eligibility Issues
If Medicaid coverage recently lapsed, plans changed, or you moved, the system may temporarily show you as ineligible.
What to Do First After a Denial
Before appealing, the first key step to take is to confirm why the denial happened. To do that, here’s what to request from Medicaid:
- The denial letter or explanation of benefits (EOB)
- The denial reason code or written explanation
- Whether the denial came from Medicaid or the managed care plan
Understanding the underlying cause of the denial can start to highlight the best-possible resolutions and path forward.
How the Medicaid Appeal Process Works
If Medicaid or your plan denies coverage, you have the right to appeal. This process typically moves forward with the following steps.
Step 1: File an Appeal Within the Deadline.
In Washington, Oregon, and Idaho, Medicaid generally provides a 30-to 60-day period from the denial notice date to file an appeal, depending on the state and managed care plan. Always review your denial letter carefully to confirm your exact deadline and submission method.
Appeals are typically filed with your Medicaid managed care plan first, and if the denial is upheld, you may then request a state fair hearing through your state’s Medicaid agency.
 In many cases, appeals can usually be submitted:
In many cases, appeals can usually be submitted:
💻 Online
📬 By mail
📞 By phone
Step 2: Include the Required Supporting Documentation.
This documentation generally includes (and may not be limited to):
- An updated prescription
- Medical records supporting the diagnosis
- A letter of medical necessity (if available)
- Any prior authorization paperwork
Step 3: Request Continuation of Benefits (When Applicable).
If you previously received free incontinence supplies through Medicaid, you may be able to request continued coverage during the appeal.
Step 4: Await a Decision.
Most appeals are reviewed within 30 to 45 days, with decisions issued by mail. In some cases, urgent medical appeals may be expedited.
4 Doctor Documentation Fixes That Often Lead to Approval
Small changes in documentation can frequently turn denials into approvals. These often involve the following updates and details.
1. Use a Specific Diagnosis.
 Rather than describe symptoms or generic issues, specific diagnoses should be documented and shared with Medicaid for review and approval. Examples include (and are not limited to):
Rather than describe symptoms or generic issues, specific diagnoses should be documented and shared with Medicaid for review and approval. Examples include (and are not limited to):
- Urinary incontinence
- Fecal incontinence
- Mixed incontinence
- Neurogenic bladder
- Functional incontinence
2. Avoid vague terms, like “leakage” or “bladder problems.”
Severity and frequency should be well documented, with statements like the following typically serving as strong indicators of medical necessity:
- Patient experiences daily urinary incontinence
- Requires protection day and night
- Stress urinary incontinence requires 6 adult diapers/day and 3 at night.
3. Clearly State Product Type
It’s not enough for documentation to affirm that you need “incontinence supplies.” Exactly what you need should be listed in detail. For example, that could include (and may not be limited to):
- Disposable briefs
- Protective underwear (pull-ups)
- Booster pads
- Underpads
4. Match Quantity to Medical Need
If higher quantities are required, the provider should document why. If quantities over the set monthly maximums are needed, the provider will generally need to initiate a prior authorization on your behalf.
Resubmitting Your Request Successfully
 After documentation has been reviewed and corrected, it’s crucial to:
After documentation has been reviewed and corrected, it’s crucial to:
- Obtain an updated prescription.
- Confirm the diagnosis and quantities required.
- Work with a healthcare provider to submit a prior authorization, if required.
- Resend the complete packet to the supplier or Medicaid for review.
A properly assembled submission can dramatically improve approval odds.
Washington, Oregon & Idaho Medicaid Notes
While each state administers Medicaid differently, these rules and requirements generally apply across Washington, Oregon, and Idaho Medicaid programs.
| State / Program | Coverage Requirements | Additional Notes |
|---|---|---|
| Washington (Apple Health) | Prescription + medical necessity required | Quantities must align with diagnosis; managed care plans may impose additional steps |
| Oregon (OHP) | Prior authorization often required | Diagnosis-specific coverage rules; plan-level review common |
| Idaho Medicaid | Prescription + medical necessity required | Quantity limits enforced; appeals available through state Medicaid or plan |
Because plan rules change, working with a supplier that verifies coverage before submission can be the key to reducing the risk of denials.
When a Denial Doesn’t Mean “No”
In most cases, a denial means:
- Something was missing
- Something was coded incorrectly
- Something exceeded limits
It rarely means you are permanently ineligible.
How MyMedSupplies Helps After a Denial

MyMedSupplies works with Medicaid beneficiaries in Washington, Oregon, and Idaho to
- Review denial reasons.
- Verify eligibility.
- Request corrected prescriptions.
- Handle documentation.
- Submit or resubmit requests.
This can remove the guesswork and shorten approval time.
When Medicaid Denies Diaper Coverage: Next Steps
A Medicaid denial can feel overwhelming, but it is often a solvable paperwork problem, not a dead end. With the right diagnosis, documentation, and submission process, many denied requests are later approved.
If your Medicaid request for incontinence supplies was denied, MyMedSupplies can help you understand why and guide you through the next steps.